 In April, the drug erdafitinib (Balversa) became the first therapy targeting a genetic alteration to be approved by the Food and Drug Administration (FDA) to treat patients with metastatic urothelial carcinoma, the most common type of bladder cancer.
In April, the drug erdafitinib (Balversa) became the first therapy targeting a genetic alteration to be approved by the Food and Drug Administration (FDA) to treat patients with metastatic urothelial carcinoma, the most common type of bladder cancer.
FDA granted an accelerated approval to the drug, which blocks the activity of a family of proteins called fibroblast growth factor receptors (FGFR), for patients with specific FGFR gene alterations, based on preliminary data from a clinical trial.
New findings from that trial have just been published. The updated results confirm that erdafitinib can benefit patients with advanced bladder cancer whose tumors have a genetic alteration in one of the four FGFR genes, according to Arlene Siefker-Radtke, M.D., of the University of Texas MD Anderson Cancer Center, who led the trial.
In the study, erdafitinib decreased the tumors of some patients whose cancers did not respond to other treatments, the researchers reported in the New England Journal of Medicine on July 25.
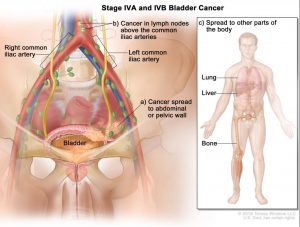
FDA’s approval covers patients whose cancer has spread outside of the bladder locally or to other parts of the body during or after treatment with standard chemotherapy.
“Our patients with metastatic bladder cancer have very limited treatment options, and this represents a real unmet need,” Dr. Siefker-Radtke said.
“Now that erdafitinib has been approved by the FDA, doctors can incorporate the drug into treatment strategies to benefit patients with FGFR-altered urothelial cancer,” she continued. “Additional research is ongoing to learn how to combine erdafitinib with immunotherapy drugs such as immune checkpoint inhibitors.”
FDA has approved several checkpoint inhibitors for advanced bladder cancer, but only approximately 20% of patients benefit from these treatments, Dr. Siefker-Radtke noted.
By comparison, 40% of the patients in the international phase 2 trial that led to the approval responded to erdafitinib, Dr. Siefker-Radtke and her colleagues reported.
To confirm the study’s results, a phase 3 clinical trial is comparing erdafitinib with standard chemotherapy and with the checkpoint inhibitor pembrolizumab (Keytruda) in patients with advanced bladder cancer whose tumors have an FGFR alteration.
Clinical Trial Results
Approximately 20% of patients with metastatic urothelial cancer of the bladder and 35% of patients with metastatic urothelial cancer of the renal pelvis and ureter have an alteration in an FGFR gene. When FDA approved erdafitinib, which is given as a pill, the agency also approved a companion diagnostic test that doctors can use to help identify patients whose tumors carry one of these FGFR alterations.
Of the 99 patients in the trial, 87 had been treated previously with chemotherapy, and 43% had received at least two prior courses of treatment. Nearly 80% had metastases beyond nearby lymph nodes.
“Overall, this group of patients typically has poor outcomes,” said Dr. Siefker-Radtke.
For this reason, a 40% response rate is “really remarkable,” noted Andrea Apolo, M.D., of NCI’s Center for Cancer Research, who was not involved in the trial.
“Erdafitinib is an important new drug for some of our patients with bladder cancer,” she added.
In the trial, the median amount of time before the disease progressed (progression-free survival) was 5.5 months, and the median overall survival was 13.8 months.
The most common treatment-related side effects included inflammation or irritation of the mucous membranes in the mouth, changes to nails, and hand–foot syndrome.
Erdafitinib can also cause eye disorders that can lead to changes in the visual field, although these can be managed, according to Dr. Siefker-Radtke.
In the trial, 46% of patients experienced side effects that were largely managed by adjusting the dose of therapy. Thirteen percent of the patients discontinued treatment because of side effects.
Janssen Research & Development, which developed erdafitinib in collaboration with Astex Pharmaceuticals, sponsored the trial.
Rapid Responses to Treatment
For some patients in the trial, tumors started responding to erdafitinib soon after their treatments began, Dr. Siefker-Radtke noted.
“I was surprised by how quickly some patients with rapidly progressing disease responded to the drug,” she said. “Within a week or two of starting treatment, the health of some of these patients improved significantly.”
For one group of patients—those whose cancers did not respond to immunotherapy drugs—the response rate was 59%, suggesting to the researchers that these patients, in particular, might benefit from erdafitinib.
In previous bladder cancer clinical trials, Dr. Siefker-Radtke had noticed that patients with FGFR mutations were less likely to respond to checkpoint inhibitors than patients who lacked the mutations.
When erdafitinib became available, she and her colleagues developed the phase 2 trial. But the current results are not definitive, Dr. Siefker-Radtke cautioned.
The phase 3 trial, she added, will provide more information about “whether patients with FGFR-altered urothelial cancer benefit more from erdafitinib or a checkpoint inhibitor.”
Source: National Cancer Institute
Categories: NEWS

