 Chaos can be surprisingly orderly. While cancer is characterized by uncontrolled cell growth, that growth is, nevertheless, the result of a very particular cascade of events, from carcinogen exposure to genetic mutations. Interfere with that cascade, and cancer can be ground to a halt, or even killed off. The efforts of longtime NFCR-supported research luminary, Harold Dvorak, M.D., help reveal this—specifically, his work with a particular protein.
Chaos can be surprisingly orderly. While cancer is characterized by uncontrolled cell growth, that growth is, nevertheless, the result of a very particular cascade of events, from carcinogen exposure to genetic mutations. Interfere with that cascade, and cancer can be ground to a halt, or even killed off. The efforts of longtime NFCR-supported research luminary, Harold Dvorak, M.D., help reveal this—specifically, his work with a particular protein.
“It’s a growth factor made by tumor cells but also has a very important role in wound healing,” Dr. Dvorak explains, speaking of the protein. “And, in fact, what tumors do by making VEGF is mimicking wound healing. Tumors become wounds that do not heal.”
His discovery of VEGF, which in 2006 garnered Dr. Dvorak the inaugural Szent-Györgyi Prize for Progress in Cancer Research, is an exquisite example of the paradigm shift oncology is currently experiencing: a move from what cancer is to discovering why cancer does what it does. And an entire category of effective, powerful and commonly used anti-cancer drugs are rooted in this NFCR-supported discovery.
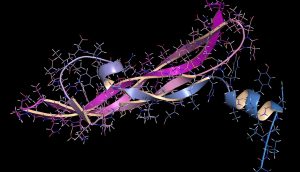
VEGF is short for “vascular endothelial growth factor,” and comes in forms A, B, C and D. This family of proteins is an absolutely vital part of bodily growth, being responsible for the formation of the embryonic circulatory system, the development of lymphatic vasculature and, perhaps most importantly, the growth of blood vessels from pre-existing vasculature, which is essential to wound healing. While it is vital to the health of the body, too much of it leads to problems down the line.
In order to grow from a single, mutated cell, cancer has to hijack standing biological systems in order to support itself. Indeed, it creates its own rooting and connective tissue, known as stroma.
With financial backing from NFCR commencing in 1980, Dr. Dvorak sought out to understand how stroma developed. He observed that one component of a tumor’s connective tissue was a then-unidentified protein, normally found in blood, that made vessels “leaky.” Seepage induced new vessel formation. He suspected that there had to be something the tissues were making in order to cause this leaking, which was creating stroma.
Indeed, as his research soon uncovered: There was! VEGF was the protein, and his discovery of it in 1983 was a huge leap for oncology.
“Stroma is the supportive connective tissue; all tissues in the body need stroma,” Dr. Dvorak explains. “Tumors need blood vessels to survive and grow. And so, what VEGF does is induce the formation of stroma and new blood vessels. If you block VEGF, you block new blood vessel formation, thereby starving tumors.”
Based on this principle, cancer drugs like bevacizumab, sold under the trade name Avastin® and first approved by the U.S. Food and Drug Administration in 2004, bind to VEGF and render it inert. Without this critical chemical signaling device, its roots whither and a tumor cannot get the nutrients it needs to grow. Indeed, it cannot even begin to do so (or continue to do so).
Avastin is currently approved for the treatment of non-small cell lung cancer, renal cell carcinoma, the aggressive brain cancer glioblastoma multiforme and certain types of cervical and ovarian cancers. Neutralizing VEGF has become such a powerful tool, that today, Avastin is applied to even non-cancerous conditions: The drug has been shown effective in slowing the effects of age-related macular degeneration and other diseases of the eye where a proliferation of blood vessels is the cause.
At the origin of Avastin and other VEGF-targeting drugs’ development and widespread use lies the willingness of NFCR to first fund research into a hunch. This hunch, well-reasoned and valid, bore out. Nearly four decades later, it has improved the lives of millions of cancer patients.
References:
- NFCR thanks Dr. Dvorak for his Spring 2019 interview
Categories: NEWS

